SWAVE 2.0: Multiparametric Imaging for Placenta Tissue Characterization
Placental insufficiency is associated with both macro- and microstructural changes in placental tissue.
Most of the current screening tests are focused on the determination of fetal size, placental structure
and depth of invasion, and other fetal-maternal responses. A more effective approach, as suggested by
recent investigations, would be to characterize and identify changes in placenta tissue as a
pathophysiological consequence of placental insufficiency. At BC Women's Hospital, We, a team consisting of two
graduate students, a pathologist, an ultrasonographer, a radiologist, and an obstetrician, are conducting a project
SWAVE 2.0 for placental tissue characterization using standard ultrasound, elastography and MRI imaging modalities,
and validation based on histopathological evaluation.
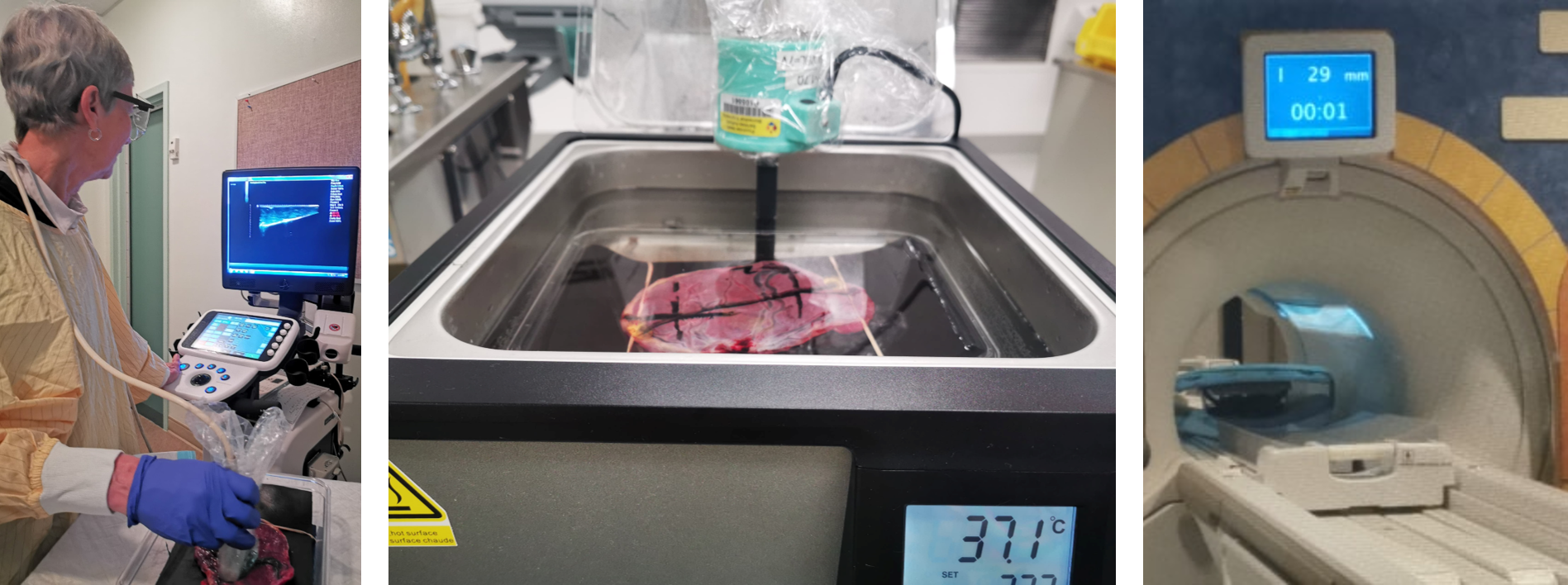 The study is designed to include ex-vivo placentas from normal singleton pregnancy (n = 10), normal twin pregnancy
(n =10), and pre-eclampsia and intrauterine growth restriction (n = 40) affected pregnancy. An experienced sonologist
locates a homogeneous and an inhomogeneous region in the placenta and mark the locations. Ultrasound B-mode images,
SWAVE elastography images [1], and MRI images are acquired from the placenta at
the marked locations. Afterwards, each placenta is examined, sampled and imaged by an experienced perinatal pathologist.
The ultrasound radio-frequency data acquired during SWAVE are utilized to compute quantitative ultrasound (QUS)
parametric images, e.g. attenuation coefficient and backscatter coefficient. Elasticity images, i.e., Young Modulus and
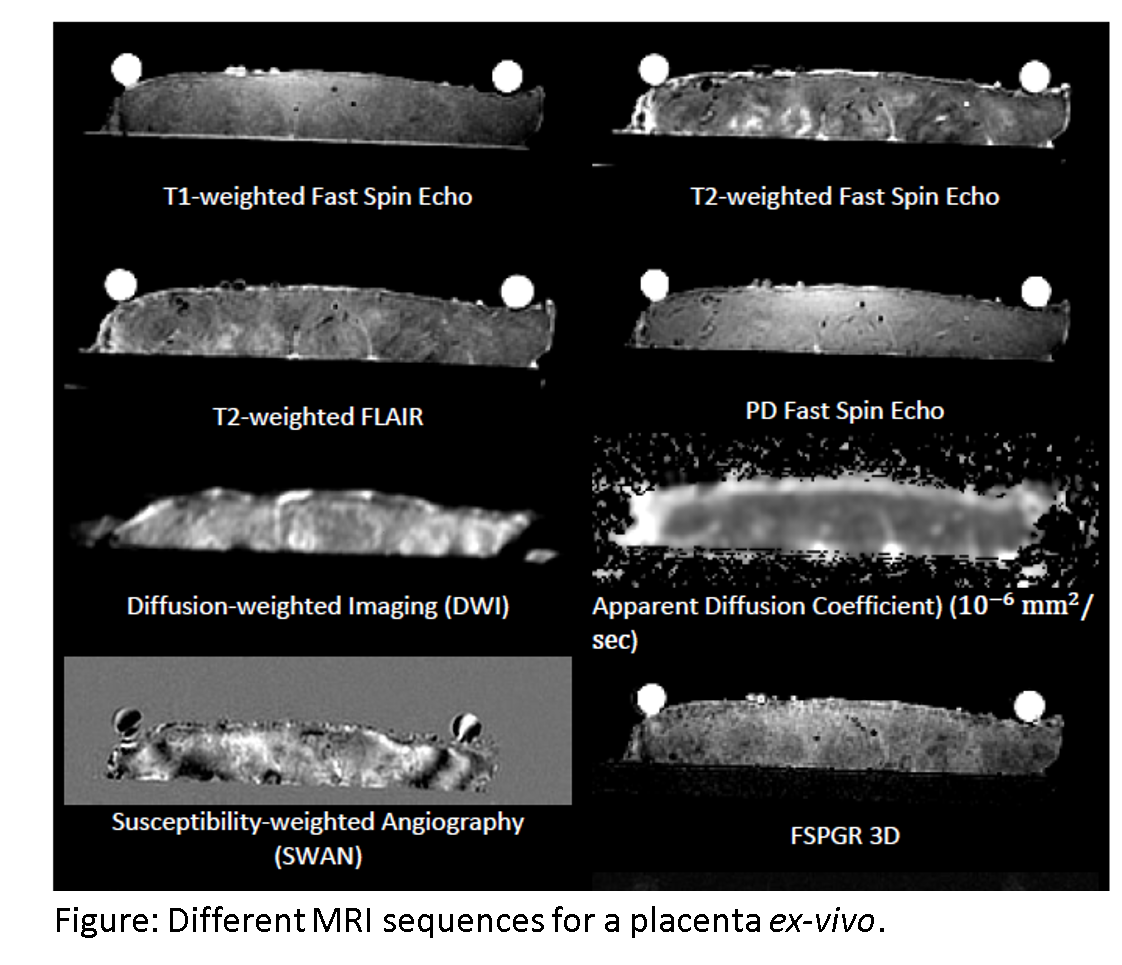
shear wave speed images will be computed from the SWAVE data. For MRI, we will use T1-weighted fast spin echo (FSE), T2-weighted
fast spin echo (FSE), T2- weighted Fluid attenuation inversion recovery (FLAIR), PD (proton density) FSE, susceptibility weighted
angiography (SWAN), and diffusion weighted imaging (DWI) sequences along with spoiled gradient-echo recalled (SPGR) sequence. The
SPGR sequence will be used for proton density fat fraction (PDFF) computation in placenta [2], which might be useful to detect
increased lipid content in complicated pregnancies [3].
The study is designed to include ex-vivo placentas from normal singleton pregnancy (n = 10), normal twin pregnancy
(n =10), and pre-eclampsia and intrauterine growth restriction (n = 40) affected pregnancy. An experienced sonologist
locates a homogeneous and an inhomogeneous region in the placenta and mark the locations. Ultrasound B-mode images,
SWAVE elastography images [1], and MRI images are acquired from the placenta at
the marked locations. Afterwards, each placenta is examined, sampled and imaged by an experienced perinatal pathologist.
The ultrasound radio-frequency data acquired during SWAVE are utilized to compute quantitative ultrasound (QUS)
parametric images, e.g. attenuation coefficient and backscatter coefficient. Elasticity images, i.e., Young Modulus and
shear wave speed images will be computed from the SWAVE data. For MRI, we will use T1-weighted fast spin echo (FSE), T2-weighted
fast spin echo (FSE), T2- weighted Fluid attenuation inversion recovery (FLAIR), PD (proton density) FSE, susceptibility weighted
angiography (SWAN), and diffusion weighted imaging (DWI) sequences along with spoiled gradient-echo recalled (SPGR) sequence. The
SPGR sequence will be used for proton density fat fraction (PDFF) computation in placenta [2], which might be useful to detect
increased lipid content in complicated pregnancies [3].
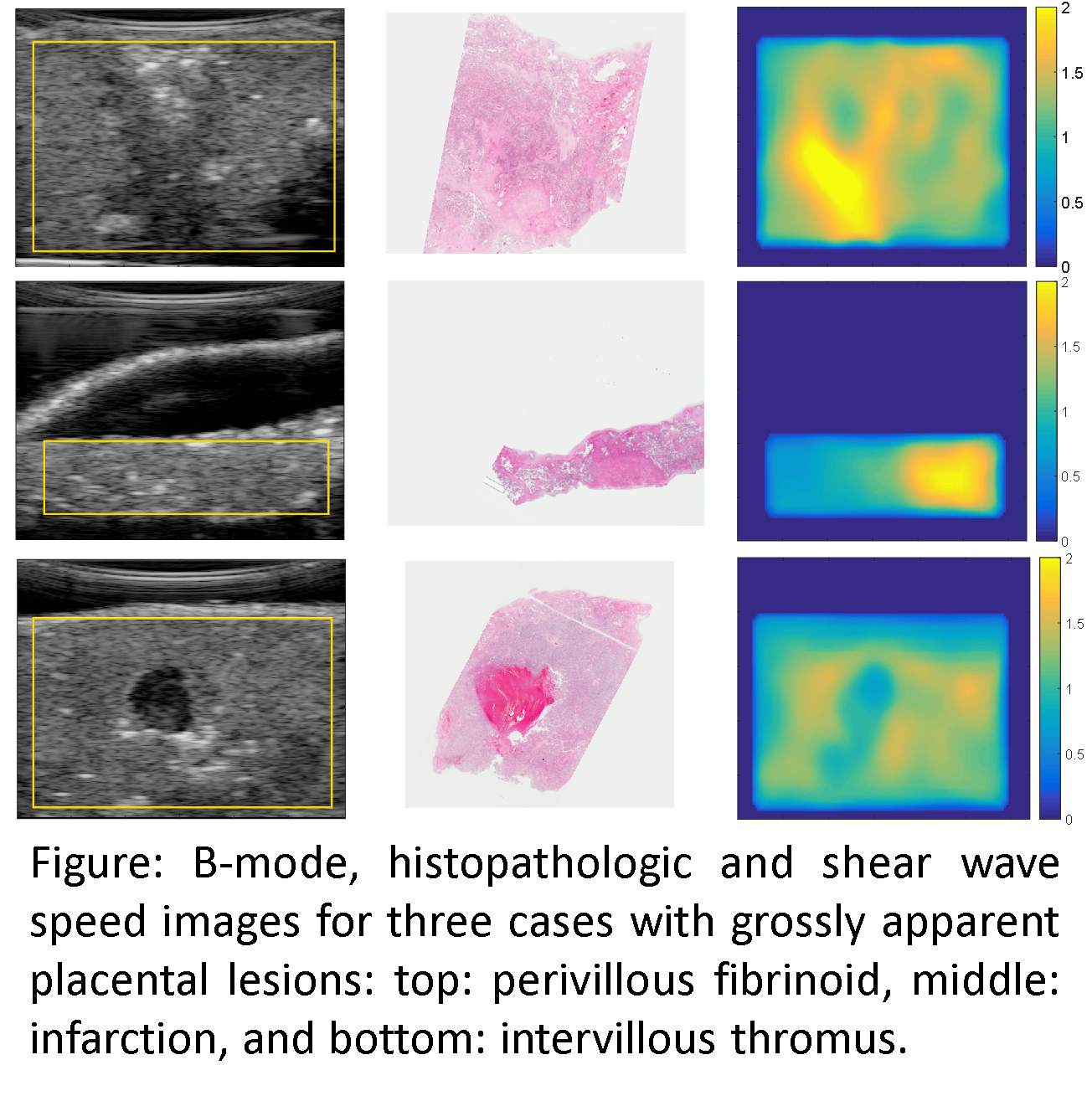
Initial results show that shear wave speed map correlates to the local structures in histological and B-mode images. Specifically,
We found distinguishable local elasticity characteristics for the following lesions: retroplacental thrombus, perivillous fibrinoid,
infarction, and intervillous thrombus. Future work involves development of non-invasive biomarkers based on the multiparametric placental
tissue characterization framework, which would be indicative of placental function. Extensive ex vivo and in vivo studies on placentas
would be performed to validate the feasibility of the developed multiparametric screening system.
1. Abeysekera, Jeffrey M., et al. "SWAVE imaging of placental elasticity and viscosity: proof of concept." Ultrasound in Medicine and Biology 43.6 (2017): 1112-1124.
2. Liu, Chia-Ying, et al. "Fat quantification with IDEAL gradient echo imaging: correction of bias from T1 and noise." Magnetic resonance in medicine 58.2 (2007): 354-364.
3. Brown, Simon HJ, et al. "A lipidomic analysis of placenta in preeclampsia: evidence for lipid storage." PloS one 11.9 (2016): e0163972.